A cervical epidural injection is a safe and effective minimally invasive treatment for neck pain. This type of spinal injection made in the neck region serves two purposes: (1) it reduces nerve inflammation, calms symptoms, aids healing and, (2) it provides important diagnostic information.
The procedure involves injecting a corticosteroid into the epidural space. A corticosteroid is a powerful, slow-releasing, and long-lasting anti-inflammatory medication effective in reducing inflammation. Sometimes a narcotic is also injected to increase pain relief. The epidural space is between the protective membrane (dura mater) covering the spinal cord and the bony spinal canal. After the medication is injected, it flows and coats the nerve roots.
Diagnostically, when the patient’s symptoms are relieved, the injection provides evidence that a particular nerve root is a pain generator.
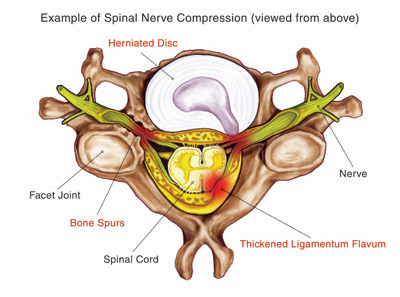
There are many spinal problems that can cause nerve irritation in the neck. As depicted in the illustration, a herniated disc or bone spurs (osteophytes) can compress fragile spinal nerve roots.
Basics about Cervical Spinal Nerves
In the cervical spine (the spine around the neck region) there are eight pairs of spinal nerves. Each pair of nerves provides sensation and function to parts of the body. Just as the levels of the cervical spine are abbreviated, the spinal nerve pairs are numbered in a corresponding way. C1 is the area between the skull and first cervical vertebra (also abbreviated C1). C8 exits the spinal canal between the last cervical vertebra (C7) and the first thoracic vertebra (T1).
Each pair of nerve roots exit the spinal column and branch out into the body forming the peripheral (outer) nervous system. These nerves innervate the upper part of the body and enable movement (motor function) and feeling (sensory function). The illustration depicts this pattern called dermatomes. The physician can use the dermatomal pattern to help diagnose the location of spinal problem based on where the patient reports pain or weakness.
Based on symptoms, medical history, physical and neurological examination, and imaging study findings (X-ray, MRI), the physician determines which spinal nerve root(s) may be generating pain and other symptoms.
Patient Procedure Preparation
In advance of the procedure, patients will be asked which medications they take. Certain drugs must be stopped several days before the procedure. In some cases, the physician may ask the patient to cease taking pain and anti-inflammatory medications in order to see how much pain relief can be attributed specifically to the epidural injection.
Possible Risks and Complications
Any medical procedure carries with it some inherent risk. Rare but serious complications include bleeding, infection, nerve injury, headache, and allergic reaction to medication. Other risks include an increase in pain, injection site tenderness, and steroid side effects. The physician will discuss the risks and benefits of this procedure with the patient.
What to Expect: The Procedure and After
The procedure is performed in an operating room, but the patient is awake. The patient, in a hospital gown, is given an intravenous line through which medications are given to keep the patient calm. During the procedure, the patient may be asked questions by the doctor to help guide the procedure. The patient is typically seated in a chair or positioned in a bed in such a way that gives the physician good access to the back of the neck. Next, the skin area is cleaned with a sterile soap. A local anesthetic is injected and given time to numb your skin and spine muscles.
The C-arm of the fluoroscope (named for its characteristic C-shape) is positioned over the patient. A fluoroscope is a type of video X-ray that projects images of the patient’s spine on monitors in the procedure room. The physician uses fluoroscopy as he injects the needle into the neck and injects a small amount of contrast (dye). This dye is injected to confirm that the needle is in the right area. Next, an anesthetic and corticosteroid is injected into the epidural space. Sometimes, pain is temporarily increased during the injection. The patient may be asked about pain. When the injection is complete, a small bandage covers the injection site.
Cervical epidural injections may require one or more injections. The entire procedure lasts about 15 minutes but may take longer if several injections are required. When it is over, the patient is moved to a recovered area and is monitored by a nurse. Upon discharge, the patient is given written instructions for home care.
Some patients experience discomfort after the procedure for two or three days. This is normal and does not necessarily mean the corticosteroid is not taking effect.
The physician’s office typically contacts the patient the day after the procedure for follow up. Patients may be asked to record their pain levels and other symptoms following the procedure because such a pain diary can assist the physician in fine-tuning future pain treatments.
Conclusion
Cervical epidural injections have provided significant pain relief to many people with moderate to severe chronic neck pain. However, epidural injections are not appropriate for all patients.